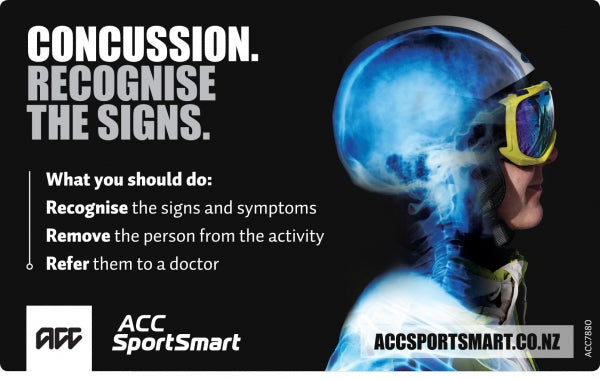
Concussion. Recognising the Signs Starts With You.
The following information has been provided by ACC SportSmart.What is concussion?
Concussion is a brain injury that can occur in any sport, particularly where there is body contact. Concussion is caused by the impact of force (a blow) to a part of the body not necessarily the head. All concussions are serious. Extra caution is required for child and adolescent athletes.
A successful recovery from a concussion starts with you recognising the signs. Only 10-20% of athletes lose consciousness. It may take several hours (or even days) post injury for some or all of the symptoms of concussion to emerge.
If concussion is suspected, remove from play or activity immediately and seek urgent assessment by a medical doctor. Diagnosis can be very difficult to make and only a medical doctor can diagnose or exclude a concussion.
What should you do?
Recognise the signs and symptoms of concussion.
Remove the athlete from play.
Refer them to a medical doctor for assessment.
Recognise the signs and symptoms of concussion.
Concussion comes with a range of signs and symptoms that may or may not include loss of consciousness.
Concussion should be suspected if one or more of the following signs or clues are present:
The following information is based on information provided from the Pocket Concussion Recognition ToolTM.
Physical signs (what you see)
• Loss of consciousness or non-responsive
• Lying on the ground not moving or slow to get up
• Loss of balance or co-ordination
• Dazed or vacant look
• Disorientated or confused
• Visible injury to face or head (especially in combination with any other signs)
• Grabbing or clutching head
Memory (what they say) Failure to answer any of these questions correctly could suggest concussion.
• “ What venue are we at today?”
• “ Which half/quarter is it now?”
• “ Who scored last in this game?”
• “ What team did you play last week?”
• “ Did your team win the last game?”
Clinical symptoms (what they feel)
• Blurred vision
• Neck pain
• Nausea
• Dizziness
• Confusion
• Sensitivity to light or noise
• Nervous or anxious
• Headache or pressure in the head
• Tired
• Irritability
• Drowsiness
• More emotional
• Problems with memory
• Reduced ability to think or concentrate
• Difficulty sleeping
Red Flags (what requires hospitalisation) If no qualified medical professional is available, consider transporting by ambulance for urgent medical assessment.
• Complaints of neck pain
• Increased confusion or irritability
• Repeated vomiting
• Seizure or convulsion
• Muscle weakness, tingling or burning in arms or legs
• Double vision
• Deterioration of conscious state
• Severe or increasing headache
• Unusual behaviour change
Concussion comes with a range of signs and symptoms
If a concussion may have occurred, non-medical people should take responsibility for removing the injured athlete from the sport or activity. If uncertain, always adopt a conservative approach – “If in doubt sit them out”.
To help an unconscious athlete:
• Apply first aid principles: DRSABC (Danger, Response, Send for help, Airway, Breathing, Circulation).
• Treat as though they have a neck injury.
• ONLY be moved by a medical professional trained in spinal immobilisation techniques.
• Do not remove helmet (if present) unless trained to do so.
• Call 111 if there is concern regarding the risk of structural head or neck injury.
An athlete with any of the following should be referred to hospital urgently:
• Complaints of neck pain.
• Increased confusion, irritability, or unusual behaviour change.
• Repeated vomiting, seizure or convulsion.
• Double vision, severe or increasing headache.
• Muscle weakness, tingling or burning in arms or legs.
• Deterioration of conscious state.
Refer them to a medical doctor for assessment
Anyone with a suspected head injury needs to be assessed by a medical doctor. Only a qualified medical doctor can assess and diagnose a concussion. This is essential to confirm the diagnosis of concussion and to assess the risk for more serious injury.
It is useful to have a list of local medical doctors, concussion clinics and emergency departments close to where the sport/ activity is being played. A checklist of the appropriate services could include:
• Local medical doctors or medical centre.
• Local hospital emergency department.
• Ambulance services (111).
What happens next: rest, recover and return
It is unanimously agreed that no return to sport/ activity on the day of concussive injury should occur.
Return to school or work may need to happen gradually and the demands altered as guided by an experienced medical practitioner.
Return to school or work and social activities should be achieved before returning to work or physical activity.
Rest until symptom-free The beginning of concussion management is about physical and mental rest until the serious symptoms clear.
Recover by following doctor’s advice and gradually becoming active Recovery involves a graduated return to activity protocol guided by a person trained in concussion management (such as a coach, trainer, teacher or parent), and under the supervision of a medical doctor. Athletes should have fully returned to school or work and social activities before returning to physical activity.
Return to sport when fully recovered & cleared by your medical doctor Clearance by a medical doctor is required before returning to your sport or activity. Following is an example of a graduated return to sport protocol based on the best available evidence and expert experience.
Graduated return to sport protocol
Return to activity stage
Functional exercise at each stage of rehabilitation
Objective of each stage
Symptom- limited activity
Daily activities that do not provoke symptoms.
Gradual reintroduction of work/school activities.
Light aerobic exercise
Keep a low or easy intensity of walking, swimming or stationary biking. No resistance training.
Increase heart rate.
Sport specific exercise
Incorporate running drills, but no head impact activities.
Add movement.
Non-contact training drills
Progress to more complex training drills e.g. passing drills.
Exercise, co-ordination and cognitive load.
Full contact practice
Following clearance from medical doctor, participate in normal training activities.
Restore confidence and assess functional skills by coaching staff.
Return to play. Resume normal sport. Full return to sport.
It is unanimously agreed that no return to sport/activity on the day of concussive injury should occur.
It is important to note that different sports have different rules and return to play guidelines. Each individual international sports federation may have specific rules which must be considered (eg International Rugby Board rules for New Zealand Rugby). Before returning it is important to check with your sports code on the rules for your sport.
Return to activity should be particularly cautious where children and adolescents are concerned.
The safety of the athlete is the priority and must NOT be compromised.
The decision to return to school, work or restricted activity should always be made by a medical doctor.
The decision of the timing to return to sport or activity should always be made by a medical doctor.
In some cases, concussion symptoms may be prolonged or graded activity may not be tolerated. Evaluation by a concussion specialist or clinic may be needed to determine if there are other aspects that could respond to rehabilitation.
REFERENCE
1. McCrory P, Meeuwisse WH, Aubry M et al. Consensus
statement on concussion in sport: The 5th International Conference on Concussion in Sport held in Berlin, October 2016. British Journal of Sports Medicine. 2017.












